Anesthesia – Keeping The Big Sleep Safe
Few things make owners as nervous as anesthesia. Heck, when I was first unleashed upon the world as “Dr. Rowland” anesthesia wracked my nerves way more than surgery. I distinctly remember the first time I knocked a patient out – I calculated the dose, double-checked it, then looked it up and checked it again, then read the drug monogram for the Nth time and checked the dose several more times. I’ve gotten over that, of course. Wouldn’t see many patients at that rate!
Here’s the thing – with the right drugs, good monitoring, and a relatively healthy patient anesthesia is quite safe. But anesthesia is never without risk, and should never be taken lightly. Today’s article is geared toward relieving the anxiety most of us feel when our pets need to be anesthetized – by giving you knowledge about what the risks really are, and what we (vets and owners) can do to minimize them.
Monitoring
Guess what the best way to miss a problem is? Not looking for it.

Anesthetic drugs don’t just cause loss of consciousness – they may affect heart rate, blood pressure, respiration and more. In case you don’t know, these things are kind of important. The body has needs – nutrients, oxygen, and removal of waste products produced by using those things. Respiration and circulation are how the body gets it done. So it only makes sense to closely monitor how all that’s working, right? And since a living body is a pretty complicated bugger, there are many things that can go wrong and many things we can watch to recognize problems and address them before they get out of hand. Here’s what I consider minimum monitoring for most procedures:
- Heart rate and blood pressure – These are the main determinants of blood flow, but they can also clue us in on “depth” of anesthesia and even other problems like blood loss.
- Electrocardiogram (ECG) – That’s the green wave with the reassuring beep on the TV hospital shows. The heart is a complicated pump running on electricity; an ECG looks at that electricity to identify problems with rate, rhythm, or coordination of the heart.
- Respiratory rate and blood oxygenation – Blood flow to your pet’s tissues does little good if it doesn’t have oxygen. And, even if you are breathing, lung or circulation problems can keep the body from getting the oxygen it needs.
Except for pulse and respiration, all those require special equipment to monitor. But this belies an important question – who monitors the monitors? Indeed, the most important monitor of all is the human being keeping track of, interpreting, and responding to all this information. Since the veterinarian is usually kind of busy -cutting this, stitching up that, and keeping sterile all the while – the best monitor is a living, breathing, highly-trained veterinary technician. They keep an eye on all that data for problems, address the minor stuff, and let me know when I need to stop playing with this or that organ and focus on what the rest of the patient is doing. Plus they monitor important stuff no machine can, like reflexesand gum color, and administer whatever treatment the vet deems necessary if problems do arise. How Do I Know You’re Healthy? A 2008 British study showed that anesthetic risk increased almost 7 times for patients with significant systemic disease. That’s not exactly surprising, but I’d go farther and say the most common reason for anesthetic problems in patients we think are healthy is that they aren’t healthy. Pets with early or mild disease often compensate well and show no outward problems – until we knock them out with a bunch of drugs that reduce their ability to compensate. Here’s what I recommend before any anesthetic procedure, to feel reasonably comfortable your pet is healthy:
- A Good History & Physical Exam – The importance of these can’t be overstated. Changes in appetite, activity level, urination or other behaviors are major clues to systemic problems. Likewise, many problems with the heart and lungs can be heard with a stethoscope. Some diseases leave early signs that can be seen with a good look at the eyes, skin, or mouth. And more than once I’vefelt something that shouldn’t be there in the abdomen of an outwardly normal patient.
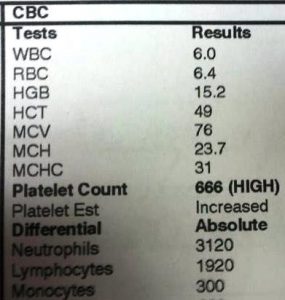
- Basic Bloodwork – Simple blood tests can identify problems with the liver or kidneys that may not cause clinical problems in your pet – until we challenge them with a bunch of anesthetic drugs. A blood count can also catch problems like anemia or inflammation, which in turn may be clues to undiagnosed infections or immune diseases.
This pet appears to be possessed by demons.
(okay, not really…)
Realistically, even if we ran thousands of dollars worth of MRI’s and fancy bloodwork we couldn’t be 100% sure your pet didn’t have some strange, subtle disease. But those simple things will rule out the majority of problems without breaking the bank – a simple blood panel runs about $40-$60 most places. Anesthetic Drugs The drugs used for anesthesia are really your vet’s prerogative, and far beyond the scope of this article. However, it’s worth briefly mentioning two things about drug choices. First off, when wedo find a health issue with a pet that requires anesthesia we use that knowledge to select the safest anesthetic drugs for the condition. Each drug has it’s own profile of side-effects that may impact the heart, liver, kidneys, etc; none are without side effects, but we can choose those least likely to aggravate the patient’s individual problems. Secondly, pain and stress also impact many of the things we worry about during anesthesia – heart rate, blood pressure, and even the heart’s electrical rhythm. While I haven’t came across any studies establishing that good pain control leads to safer anesthesia, it stands to reason that a less stressed, pain-free patient should handle anesthesia better. Most of us nowadays provide sedation prior to inducing anesthesia and various kinds of pain relief (analgesia) during procedures for just this reason. What Should You Do With This Knowledge? Here’s the point – understanding all this means you can make informed choices when your pet needs anesthesia. Here are some questions you should now be able to ask when choosing a vet for a procedure:
- What kind of things do you monitor when Muffy’s asleep?
- Is there a person watching Muffy while he’s out? What kind of training do they have?
- What kind of bloodwork do you recommend?
- Based on your exam, do you think Muffy’s okay for anesthesia? Is there anything else we should check?
- If the procedure may be painful, what kind of pain control do you provide?
- Do you have any other questions about Muffy, Doc? (That is a smart owner question.)
So, why tell you all this? Thing is, many great, smart veterinarians don’t do all the things they’d like to or feel they should because of financial reasons – that is, you won’t pay for it. Not every clinic provides all these services, and many clinics that do offer everything mentioned above make them “optional” for an additional fee. Those monitors I talked about run $3,000-$10,000, with a life expectancy of a few years. The technician monitoring the monitors is $13-25 per hour. If you won’t pay for it, we can’t pay for it – or we have to cut costs somewhere else, which isn’t good for your pet either. Honestly, I don’t put the blame for that on pet owners, but squarely on we vets – we can’t expect you to pay more if you don’t understand why the extra money is worthwhile. Hopefully now you do, and can make informed decisions about who treats your pet and how. The most expensive place in town may not necessarily be the best, but I can pretty much guarantee if you price-shop around for the cheapest place your pet is missing out on some or all of these safety measures. Likewise, some vets make good arguments that some of the things discussed here aren’t necessary. And maybe they aren’t strictly necessary – the vast majority of outwardly health animals are indeed healthy, and would probably be fine if knocked out with a 20-year old drug protocol and ignored. Bear that in mind if you truly can’t afford the extra money for all the “best” care. But most of us can handle an extra $100-150 for good monitoring, pain control, and some basic bloodwork; the peace of mind it buys is worth a lot more, if you ask me.
